Many more people could be saved from heroin and prescription opioid deaths if more frontline rescuers were trained to use the overdose reversal drug naloxone, the Centers for Disease Control and Prevention (CDC) announced. A new CDC study has found that the non-addictive prescription drug naloxone has been especially underused to reverse opioid overdoses in the country’s most rural regions. In 2013, more than 16,000 people in the nation died of prescription opioid overdose, the CDC reports, while another 8,000 died of heroin overdoses.
Rural and Urban Naloxone Disparity
Overall, the country’s opioid overdose death rate was 45 percent higher in rural areas than in urban ones, yet the use of naloxone by rural emergency medical services (EMS) staff was only 22.5 percent higher than urban counterparts, concludes the CDC study published online in April 2015 by the American Journal of Public Health. “Opioid overdose deaths are devastating families and communities, especially in rural areas,” CDC Director Tom Frieden, MD, MPH, said in announcing the new findings. “Many of these deaths can be prevented by improving prescribing practices to prevent opioid addiction, expanding the use of medication-assisted treatment, and increasing use of naloxone for suspected overdoses. Having trained EMS staff to administer naloxone in rural areas will save lives.”
What Are Opioids and Naloxone?
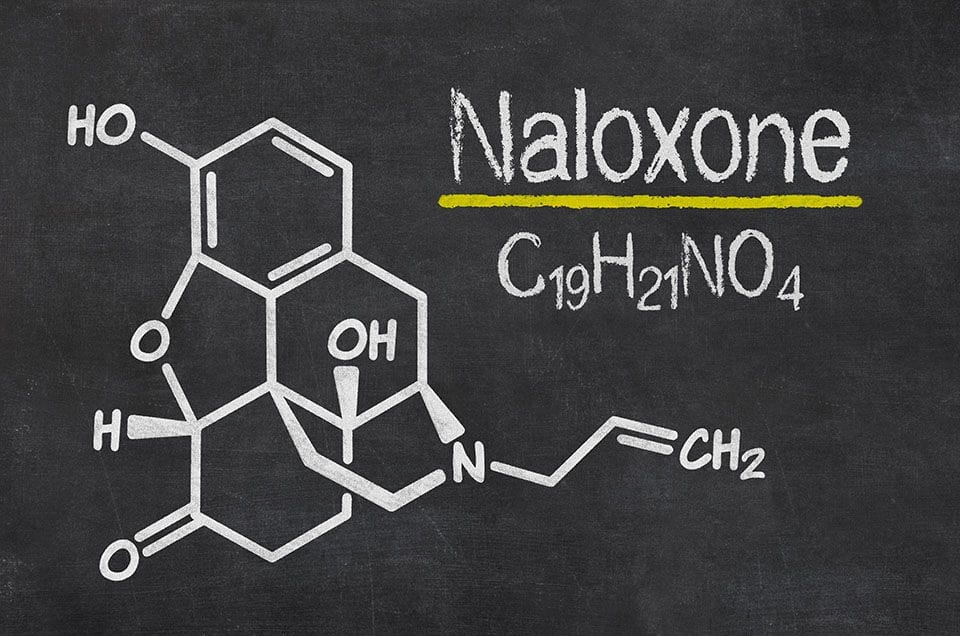
Opioids include heroin and powerful narcotic prescription painkillers such as OxyContin, Percocet, Vicodin, and codeine. Both forms of opioids are part of an alarming rise in addiction and overdoses that have been called a public health crisis. In conveying the scale to which people in the U.S. are hooked on opioids, the CDC has said that in 2010 Americans were given enough prescription painkillers to medicate every adult for a month. By all accounts, the drug naloxone is a lifesaver. It was originally given via injection, but can now be administered nasally, making it simpler for a less-trained medic. It can reverse the effects of an opiate overdose within minutes of administration by stopping potentially fatal respiratory depression. A 2010 CDC nationwide survey of 188 local prevention programs revealed that by quick injection or nasal administration of naloxone, more than 10,000 lives were likely saved between 1996 and 2010. A Call for More EMT Training in Naloxone Delivery In the newest study, researchers analyzed national data from 2012, finding that more advanced EMS personnel with training certification were more likely than basic EMS staffers to deliver naloxone to an overdose patient. That’s because only a dozen states allowed that basic level of EMS to do so. “Naloxone is non-addictive,” CDC senior health scientist Mark Faul said in a news announcement of the findings, “and expanding training on how to administer the drug can help basic emergency medical service staff reverse an opioid overdose and save more lives.” According to Addiction.com, more than 50,000 people have received training from special programs, and figures indicate that well over 10,000 cases of overdose have been successfully treated or prevented by program participants. In many of those communities with layperson naloxone training programs, there are reports of a substantial decline in fatal opioid overdoses.
Naloxone Numbers
In the CDC’s analysis titled “Disparity in Naloxone Administration by Emergency Medical Service Providers and the Burden of Drug Overdose in Rural Communities,” there were these demographic findings: The overdose reversal drug was most likely to be administered to women, to people between 20 and 29 years old, and to residents in suburban, urban and rural communities, in that order.